Retinal Tears and Detachment
 A vitreous detachment occurs suddenly without any warning. It is more common as people get older. By age 60, 90% of all people will have a vitreous detachment in at least one eye. It is so common we consider it to be a normal part of getting older. Patients that are very nearsighted have a higher chance of a vitreous detachment at a younger age, as do people who are hit in the eye or in the head.
A vitreous detachment occurs suddenly without any warning. It is more common as people get older. By age 60, 90% of all people will have a vitreous detachment in at least one eye. It is so common we consider it to be a normal part of getting older. Patients that are very nearsighted have a higher chance of a vitreous detachment at a younger age, as do people who are hit in the eye or in the head.
In some patients, the collapse of the vitreous occurs in stages rather than all at once. For that reason, the Retina Specialist will examine the patient when the symptoms first occur and then again 6 to 8 weeks later. If the floaters and flashes suddenly get worse at any time or if a grayish curtain appears in your peripheral vision, you should call the office immediately. This advice holds true if these symptoms occur in your other eye. Often, the vitreous in both eyes will detach within a year of each other.
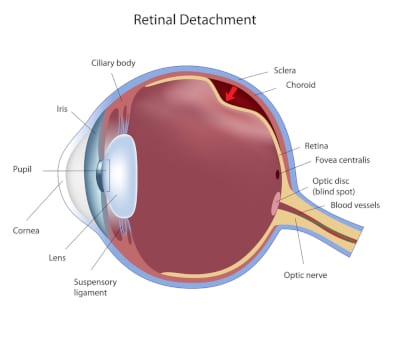
In the vast majority of patients, a vitreous detachment is annoying but not dangerous. However, in some people the vitreous gel tugs so much on the retina it causes a tear or hole to form in the retina. In many of these patients, the saltwater that is now free inside the eye can go through the hole and cause a retinal detachment. Therefore, it is imperative that all patients who experience flashes and floaters have a detailed examination of the vitreous and retina by a Retina Specialist who is an expert in this area. If a hole or tear is found in the retina, it can be easily treated using a laser. The laser seals the tear by making “spot welds” in the retina and prevents fluid from going under the retina and creating a retinal detachment. If a retinal detachment has already occurred, an operation performed by a Retina Specialist is usually required. Patients, who are at a higher risk of getting a retinal detachment, include people who are very nearsighted, those who have had a retinal hole or detachment in the other eye, or who have a family history of retinal detachment.
The main symptom of a retinal detachment is the sensation of a “curtain” coming across the field of vision from the side toward the center. The curtain gets progressively larger over several hours or days. As the detachment reaches the center of the retina (the macula), the vision becomes very blurry, often preventing the patient from seeing anything other than fingers in front of their faces. The curtain can come from any direction (left, right, top or bottom) and is related to which part of the retina detaches first. There is often a sensation of waviness, as the retina undulates because of the fluid underneath it. The flashing lights and floaters will persist during this time. A retinal detachment is a true emergency and needs to be treated as soon as possible; ideally, before it reaches the macula. Once the macula detaches and depending upon how long it is detached, the likelihood of regaining normal vision in the eye is significantly diminished.
Treatment of Retinal Tear and Detachment
Treatment of a retinal detachment depends upon several factors. There are three main procedures used to treat retinal detachments. A pneumatic retinopexy is a procedure performed in the office in which the retinal tear causing the detachment is treated with cryotherapy (a freezing probe). A gas bubble, usually perfluoropropane, is injected into the eye under sterile conditions. You will be given drops and perhaps some oral medications to take after the procedure. The most important part of a pneumatic retinopexy is the positioning the patient must maintain after the procedure. The position you will be asked to maintain depends on the location of the tear causing the detachment. For example, if you have a tear on the right side of the retina in the right eye, you will be asked to lie on your left side. The reason for this is so that the gas bubble can float to the side of the tear and seal it off, allowing the fluid under the retina to be reabsorbed over 2 to 4 days. You would then have an appointment to see the doctor and, if the retina is reattached, he will perform laser treatment to tack the retina down in the area in which it was detached. The gas bubble will reabsorb in 4 to 6 weeks. Only certain retinal detachments are eligible for a pneumatic retinopexy, usually depending on the location of the tear in the retina and the patient’s ability and willingness to maintain the positioning after the procedure. Pneumatic retinopexy has a 95% success rate.
If there is more than one tear in the retina, the tear is located at the bottom of the retina, there is too much blood in the vitreous cavity, or a significant amount of scar tissue has formed on the retina, then a pneumatic retinopexy is not a viable treatment option. In those patients, a vitrectomy is performed in the operating room. In a vitrectomy, the vitreous gel and any blood or scar tissue are removed and the retina is reattached during the procedure by aspirating the fluid from underneath the retina while simultaneously infusing air into the eye. Freezing treatment and/or laser treatment is performed to seal the tears in the retina. The air is then replaced with gas or silicone oil. The gas will reabsorb and disappear in 4 to 6 weeks. The silicone oil will be left inside the eye for 4 to 6 months, and then will be removed if the situation permits. Silicone oil is usually reserved for eyes with more severe detachments or eyes in which the retina has detached more than once or twice. Whether gas or silicone oil is used, the surgeon may ask you to lie in a certain position for several days after the surgery. Vitrectomy surgery for a primary (first) detachment has a 95% success rate, though recovery of vision may not occur for 6 to 12 months.
 Scleral buckling is a procedure performed in the operating room in which a plastic band is placed around the outside of the eye, under the four rectus muscles. It is sewn to the wall of the eye and tightened to indent (buckle) the wall of the eye. You can think of it like a belt that goes around your waist to hold up your pants. The buckle remains in place permanently. The operation requires an incision all around the skin of the eye and can result in a moderate amount of pain postoperatively. A scleral buckle may be performed as a procedure all by itself or it may be combined with a vitrectomy. Your eye surgeon will discuss these options with you and recommend the one he feels gives you the best chance of reattaching the retina.
Scleral buckling is a procedure performed in the operating room in which a plastic band is placed around the outside of the eye, under the four rectus muscles. It is sewn to the wall of the eye and tightened to indent (buckle) the wall of the eye. You can think of it like a belt that goes around your waist to hold up your pants. The buckle remains in place permanently. The operation requires an incision all around the skin of the eye and can result in a moderate amount of pain postoperatively. A scleral buckle may be performed as a procedure all by itself or it may be combined with a vitrectomy. Your eye surgeon will discuss these options with you and recommend the one he feels gives you the best chance of reattaching the retina.
The main reason for the failure of retinal detachment surgery is the formation of scar tissue, usually about 6 weeks after the procedure. This complication is called proliferative vitreoretinopathy and occurs in 3 to 5% of all eyes. There is no known way to prevent this problem. If enough scar tissue forms, it can pull the retina off the wall of the eye or cause additional holes to form in the retina. Eyes with proliferative vitreoretinopathy usually require more advanced surgery to correct the problem, usually involving a scleral buckle and silicone oil.
In summary, flashes and floaters are very common problems. Although a vitreous detachment is usually not dangerous by itself, it can have serious consequences. Therefore, call Dr. Kirsch, Dr. Hairston, or Dr. Ho immediately if you experience these symptoms. Your eyesight may depend on it.
Schedule your Retina Evaluation today
Call (727) 581-8706 to schedule your appointment
Meet Your Retina Care Specialists
 Leonard S. Kirsch, MD is a fellowship-trained vitreous and retina specialist. He is internationally known for the numerous papers and lectures he has presented here and abroad. Dr. Kirsch is currently an active participant in ongoing research to find new treatments for diseases of the retina. His expertise in the most advanced diagnostic and treatment techniques of all diseases of the retina, macula, and vitreous make Dr. Kirsch one of the elites in his field. In the Tampa Bay area, Dr. Kirsch pioneered the use of Photodynamic Therapy with Visudyne©, and intravitreal Macugen©, Lucentis©, and Avastin© for the treatment of age-related macular degeneration. Dr. Kirsch was also among the first surgeons in Florida to perform 25 gauge “no-stitch” vitrectomy in 2001. He is certified by the American Board of Ophthalmology and is a fellow of the Royal College of Surgeons of Canada.
Leonard S. Kirsch, MD is a fellowship-trained vitreous and retina specialist. He is internationally known for the numerous papers and lectures he has presented here and abroad. Dr. Kirsch is currently an active participant in ongoing research to find new treatments for diseases of the retina. His expertise in the most advanced diagnostic and treatment techniques of all diseases of the retina, macula, and vitreous make Dr. Kirsch one of the elites in his field. In the Tampa Bay area, Dr. Kirsch pioneered the use of Photodynamic Therapy with Visudyne©, and intravitreal Macugen©, Lucentis©, and Avastin© for the treatment of age-related macular degeneration. Dr. Kirsch was also among the first surgeons in Florida to perform 25 gauge “no-stitch” vitrectomy in 2001. He is certified by the American Board of Ophthalmology and is a fellow of the Royal College of Surgeons of Canada.
 Richard J. Hairston, M.D. is a vitreous and retina specialist. He joined The Eye Institute in June 2001 coming to us from a busy retina practice in Washington, DC. Dr. Hairston graduated from the Johns Hopkins University School of Medicine and did his residency at the Wilmer Ophthalmological Institute at Johns Hopkins University. He completed a fellowship in diseases and surgery of the retina and vitreous at The Center for Retina Vitreous Surgery, Memphis, Tennessee. He then served as Assistant Chief of Service in Ophthalmology and Director of the Ocular Trauma Service at Johns Hopkins Hospital. Most recently he was Assistant Professor of Ophthalmology at Johns Hopkins University. He is certified by the American Board of Ophthalmology. Dr. Hairston enjoys an international reputation as an outstanding retina and vitreous surgeon.
Richard J. Hairston, M.D. is a vitreous and retina specialist. He joined The Eye Institute in June 2001 coming to us from a busy retina practice in Washington, DC. Dr. Hairston graduated from the Johns Hopkins University School of Medicine and did his residency at the Wilmer Ophthalmological Institute at Johns Hopkins University. He completed a fellowship in diseases and surgery of the retina and vitreous at The Center for Retina Vitreous Surgery, Memphis, Tennessee. He then served as Assistant Chief of Service in Ophthalmology and Director of the Ocular Trauma Service at Johns Hopkins Hospital. Most recently he was Assistant Professor of Ophthalmology at Johns Hopkins University. He is certified by the American Board of Ophthalmology. Dr. Hairston enjoys an international reputation as an outstanding retina and vitreous surgeon.
 Janie Ho M.D., is a board-certified ophthalmologist, fellowship-trained in medical and surgical vitreoretinal diseases such as macular degeneration, diabetic retinopathy and retinal tears and detachments. She has been educated at some of America’s finest institutions. She received her Bachelor of Arts from Harvard University and her medical degree from Duke University. She went on to ophthalmology residency at the University of California, San Francisco. Following residency, Dr. Ho continued on to a fellowship in vitreoretinal diseases at the prestigious Massachusetts Eye and Ear Infirmary of Harvard Medical School. Dr. Ho has participated in angiogenesis research, investigating causes and treatment for common retinal disorders.
Janie Ho M.D., is a board-certified ophthalmologist, fellowship-trained in medical and surgical vitreoretinal diseases such as macular degeneration, diabetic retinopathy and retinal tears and detachments. She has been educated at some of America’s finest institutions. She received her Bachelor of Arts from Harvard University and her medical degree from Duke University. She went on to ophthalmology residency at the University of California, San Francisco. Following residency, Dr. Ho continued on to a fellowship in vitreoretinal diseases at the prestigious Massachusetts Eye and Ear Infirmary of Harvard Medical School. Dr. Ho has participated in angiogenesis research, investigating causes and treatment for common retinal disorders.
 Sejal Shah M.D., is a board-certified, fellowship-trained Retina Specialist. Dr. Shah received her medical degree from the University of South Florida. She began her postgraduate training with an internship in medicine at UCLA, followed by ophthalmology training at the University of South Florida. She went on to complete a fellowship at the prestigious Bascom Palmer Eye Institute, specializing in the diagnosis and treatment of retinal disorders. Dr. Shah also earned a B.S. degree with honors in Nutritional Science from the University of Florida. Dr. Shah brings her expertise as a medical retinal specialist with skills in managing and treating vitreoretinal pathology which including age-related macular degeneration and diabetic retinopathy. Her research has appeared in publications such as Ophthalmic Surgery, Lasers, and Imaging Retina; Clinical Ocular Oncology; Survey of Ophthalmology; International Ophthalmology Clinics; and Survey of Ophthalmology. In her spare time, she enjoys spending quality time with her family and friends, traveling, and trying to keep up with her twin boys.
Sejal Shah M.D., is a board-certified, fellowship-trained Retina Specialist. Dr. Shah received her medical degree from the University of South Florida. She began her postgraduate training with an internship in medicine at UCLA, followed by ophthalmology training at the University of South Florida. She went on to complete a fellowship at the prestigious Bascom Palmer Eye Institute, specializing in the diagnosis and treatment of retinal disorders. Dr. Shah also earned a B.S. degree with honors in Nutritional Science from the University of Florida. Dr. Shah brings her expertise as a medical retinal specialist with skills in managing and treating vitreoretinal pathology which including age-related macular degeneration and diabetic retinopathy. Her research has appeared in publications such as Ophthalmic Surgery, Lasers, and Imaging Retina; Clinical Ocular Oncology; Survey of Ophthalmology; International Ophthalmology Clinics; and Survey of Ophthalmology. In her spare time, she enjoys spending quality time with her family and friends, traveling, and trying to keep up with her twin boys.

