Diabetic Retinopathy
 Diabetes mellitus affects approximately 16 million Americans. Diabetes occurs in two main forms: Type I (also called juvenile-onset) in which the pancreas does not produce enough insulin for a person to live; and Type II (also called adult-onset), in which the pancreas continues to produce insulin but the cells in the rest of the body have difficulty using the insulin effectively. Patients with Type I diabetes must always take insulin, while patients with Type II diabetes may be treated with diet alone, pills, and/or insulin.
Diabetes mellitus affects approximately 16 million Americans. Diabetes occurs in two main forms: Type I (also called juvenile-onset) in which the pancreas does not produce enough insulin for a person to live; and Type II (also called adult-onset), in which the pancreas continues to produce insulin but the cells in the rest of the body have difficulty using the insulin effectively. Patients with Type I diabetes must always take insulin, while patients with Type II diabetes may be treated with diet alone, pills, and/or insulin.
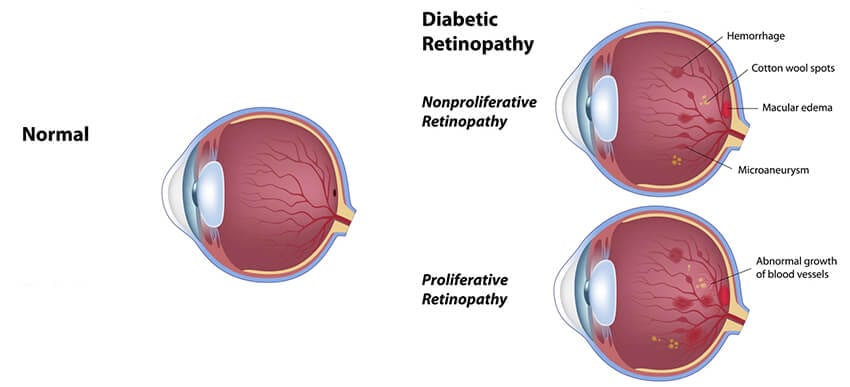
Although diabetes is a disorder of glucose metabolism, the disease affects many different parts of the body including the eyes. When diabetes affects the eyes, the most serious problems are found in the retina. This complication of diabetes, called diabetic retinopathy, is the leading cause of new blindness in the United States among people aged 25 to 64 years.
What Is the Anatomy of the Retina?
The retina is a transparent layer of tissue that lines the back wall of the eye like a piece of wallpaper on a wall. The retina functions, as does the film in a camera, to take the light coming into the eye and make a “picture” that is sent to the brain. The very center of the retina is called the macula. The macula is the part of the retina that allows the eye to have 20/20 vision. The retina is nourished by many small blood vessels that are damaged after a person has diabetes for several years, especially if the blood glucose is poorly controlled.
Proliferative Diabetic Retinopathy
In proliferative diabetic retinopathy, the blood vessels supplying the retinal tissue become so damaged they lose the ability to adequately nourish the retina. The eye responds to this situation by increasing the production of vascular endothelial growth factor (VEGF) which starts the process of growing new blood vessels. Unfortunately, these new blood vessels grow or “proliferate” (hence the term proliferative retinopathy) along the surface of the retina and do not actually meet the need for more nourishment of the retina. The abnormal new blood vessels can cause two major problems leading to loss of vision. They are very fragile and can easily break, causing hemorrhage into the large cavity in the back part of the eye. The blood vessels can also eventually form large sheets of scar tissue that can pull on the retina and lead to a retinal detachment. These two problems often have to be corrected by advanced microsurgery performed in the operating room.
How Is Proliferative Diabetic Retinopathy Treated?
The main goal of treating proliferative retinopathy is to prevent the new vessels from causing hemorrhage or a retinal detachment. This greatly reduces the risk of permanent severe vision loss, as well as, the need for major surgery. By carefully examining the retina, your surgeon can detect the new blood vessels growing on the retina before they cause a major problem. If new blood vessels are detected, laser treatment is usually recommended. The laser treatment is different than the laser performed for macular edema. In proliferative retinopathy, up to 2,000 laser spots are placed around the front part of the retina, away from the macula. This procedure is also done in the office and may be divided into two treatment sessions scheduled one week apart. Some mild discomfort may be felt for a few days afterward. The other common side effect is a mild decrease in the “side” or peripheral vision, especially at night. The new blood vessels begin to shrink within a week of the treatment. Additional laser treatment can be performed if the blood vessels don’t regress entirely or if they come back. In most patients, laser treatments cure the problem of proliferative retinopathy permanently.
 Recently, there has been a great deal of research regarding the use of medications that inhibit vascular endothelial growth factor (VEGF) to treat both macular edema and proliferative diabetic retinopathy. VEGF is a family of 6 proteins produced all over the body, including in the eye, that are critically important in the development of both normal and abnormal new blood vessels. In diabetic retinopathy, VEGF is produced in abnormally high amounts and leads to the leakiness of the macular blood vessels. This production, in turn, causes macular edema and also causes the formation of the abnormal new blood vessels that arise in proliferative diabetic retinopathy.
Recently, there has been a great deal of research regarding the use of medications that inhibit vascular endothelial growth factor (VEGF) to treat both macular edema and proliferative diabetic retinopathy. VEGF is a family of 6 proteins produced all over the body, including in the eye, that are critically important in the development of both normal and abnormal new blood vessels. In diabetic retinopathy, VEGF is produced in abnormally high amounts and leads to the leakiness of the macular blood vessels. This production, in turn, causes macular edema and also causes the formation of the abnormal new blood vessels that arise in proliferative diabetic retinopathy.
All anti-VEGF treatment is administered as an injection into the vitreous cavity, which is a procedure performed in the office. The surface of the eye is numbed with drops and then an anesthetic injection of lidocaine is given under the conjunctiva (the “skin” covering the white part of the eye). The eye is then thoroughly cleaned and sterilized with betadine and antibiotic drops. The anti-VEGF medication is injected through the anesthetized area into the vitreous cavity using a very tiny needle. The procedure itself is painless and straightforward. However, it is considered an invasive procedure because we are entering the eye itself and there is a rare chance of complications, such as cataract, retinal detachment, bleeding or infection. These complications occur less than one in a thousand injections. Occasionally, the volume of medication injected temporarily interrupts the circulation to the eye, and it might be necessary for the surgeon to remove some fluid from the front of the eye to restore the normal circulation. All patients receiving an injection are asked to take antibiotic drops for four days after the injection to lessen the chance of infection. These injections are usually repeated every 4 to 6 weeks as necessary until the problem is resolved.
There are three anti-VEGF medications that may be used to treat diabetic retinopathy: Avastin, Lucentis, and Macugen. None of these medications are approved by the Food and Drug Administration to treat diabetic retinopathy. Lucentis and Macugen are approved for treating wet macular degeneration, while Avastin is used “off-label” for all eye diseases. There has been some encouraging news lately regarding the effectiveness of these medications. In practice, Avastin is normally used because of the issues of cost; it is significantly less expensive. It is also as or more effective than either Macugen or Lucentis. Recently, there has been an indication from Medicare and other insurance companies that they will cover the cost of this treatment option for diabetic retinopathy.
Maintaining Diabetic Retinopathy
 There are two aspects of the care of diabetics which deserve special recognition. The first is the family doctor, internist, or endocrinologist responsible for managing your diabetes sends you to an ophthalmologist at least once a year for a retinal examination; if your doctor does not suggest this to you, ask him for a referral. Early detection of macular edema or proliferative retinopathy leads to a much better chance of keeping your eyesight.
There are two aspects of the care of diabetics which deserve special recognition. The first is the family doctor, internist, or endocrinologist responsible for managing your diabetes sends you to an ophthalmologist at least once a year for a retinal examination; if your doctor does not suggest this to you, ask him for a referral. Early detection of macular edema or proliferative retinopathy leads to a much better chance of keeping your eyesight.
The second issue revolves around strict control of blood sugar. The results of a study called the Diabetes Control and Complications Trial, for which Dr. Kirsch was a co-investigator, were first published in 1993. This study conclusively demonstrated that Type I diabetics, who very strictly controlled their blood glucose, had a delay in the onset of any form of diabetic retinopathy. Furthermore, if there was already some damage to the retina, the progression of retinopathy was significantly slowed by keeping the blood sugar as close to normal as possible. We now believe all diabetics should monitor their blood sugar frequently, adhere to a strict diet, exercise regularly, and try to tightly control their blood sugar levels.
While diabetes cannot be cured at the present time, it can be controlled. Most of the retinal problems caused by diabetes can be detected in the early stages and successfully treated. Working together with your primary doctor, Dr. Kirsch, Dr. Hairston, and Dr. Ho can help to preserve the precious gift of sight for a lifetime.
Schedule your Retina Evaluation today
Call (727) 581-8706 to schedule your appointment
Meet Your Retina Care Specialists
 Leonard S. Kirsch, M.D., F.R.C.S.(C) is a fellowship-trained vitreous and retina specialist. He is internationally known for the numerous papers and lectures he has presented here and abroad. Dr. Kirsch is currently an active participant in ongoing research to find new treatments for diseases of the retina. His expertise in the most advanced diagnostic and treatment techniques of all diseases of the retina, macula, and vitreous make Dr. Kirsch one of the elites in his field. In the Tampa Bay area, Dr. Kirsch pioneered the use of Photodynamic Therapy with Visudyne©, and intravitreal Macugen©, Lucentis©, and Avastin© for the treatment of age-related macular degeneration. Dr. Kirsch was also among the first surgeons in Florida to perform 25 gauge “no-stitch” vitrectomy in 2001. He is certified by the American Board of Ophthalmology and is a fellow of the Royal College of Surgeons of Canada.
Leonard S. Kirsch, M.D., F.R.C.S.(C) is a fellowship-trained vitreous and retina specialist. He is internationally known for the numerous papers and lectures he has presented here and abroad. Dr. Kirsch is currently an active participant in ongoing research to find new treatments for diseases of the retina. His expertise in the most advanced diagnostic and treatment techniques of all diseases of the retina, macula, and vitreous make Dr. Kirsch one of the elites in his field. In the Tampa Bay area, Dr. Kirsch pioneered the use of Photodynamic Therapy with Visudyne©, and intravitreal Macugen©, Lucentis©, and Avastin© for the treatment of age-related macular degeneration. Dr. Kirsch was also among the first surgeons in Florida to perform 25 gauge “no-stitch” vitrectomy in 2001. He is certified by the American Board of Ophthalmology and is a fellow of the Royal College of Surgeons of Canada.
 Richard J. Hairston, M.D. is a vitreous and retina specialist. He joined The Eye Institute in June 2001 coming to us from a busy retina practice in Washington, DC. Dr. Hairston graduated from the Johns Hopkins University School of Medicine and did his residency at the Wilmer Ophthalmological Institute at Johns Hopkins University. He completed a fellowship in diseases and surgery of the retina and vitreous at The Center for Retina Vitreous Surgery, Memphis, Tennessee. He then served as Assistant Chief of Service in Ophthalmology and Director of the Ocular Trauma Service at Johns Hopkins Hospital. Most recently he was Assistant Professor of Ophthalmology at Johns Hopkins University. He is certified by the American Board of Ophthalmology. Dr. Hairston enjoys an international reputation as an outstanding retina and vitreous surgeon.
Richard J. Hairston, M.D. is a vitreous and retina specialist. He joined The Eye Institute in June 2001 coming to us from a busy retina practice in Washington, DC. Dr. Hairston graduated from the Johns Hopkins University School of Medicine and did his residency at the Wilmer Ophthalmological Institute at Johns Hopkins University. He completed a fellowship in diseases and surgery of the retina and vitreous at The Center for Retina Vitreous Surgery, Memphis, Tennessee. He then served as Assistant Chief of Service in Ophthalmology and Director of the Ocular Trauma Service at Johns Hopkins Hospital. Most recently he was Assistant Professor of Ophthalmology at Johns Hopkins University. He is certified by the American Board of Ophthalmology. Dr. Hairston enjoys an international reputation as an outstanding retina and vitreous surgeon.
 Janie Ho M.D. is a board-certified ophthalmologist, fellowship-trained in medical and surgical vitreoretinal diseases such as macular degeneration, diabetic retinopathy and retinal tears and detachments. She has been educated at some of America’s finest institutions. She received her Bachelor of Arts from Harvard University and her medical degree from Duke University. She went on to ophthalmology residency at the University of California, San Francisco. Following residency, Dr. Ho continued on to a fellowship in vitreoretinal diseases at the prestigious Massachusetts Eye and Ear Infirmary of Harvard Medical School. Dr. Ho has participated in angiogenesis research, investigating causes and treatment for common retinal disorders.
Janie Ho M.D. is a board-certified ophthalmologist, fellowship-trained in medical and surgical vitreoretinal diseases such as macular degeneration, diabetic retinopathy and retinal tears and detachments. She has been educated at some of America’s finest institutions. She received her Bachelor of Arts from Harvard University and her medical degree from Duke University. She went on to ophthalmology residency at the University of California, San Francisco. Following residency, Dr. Ho continued on to a fellowship in vitreoretinal diseases at the prestigious Massachusetts Eye and Ear Infirmary of Harvard Medical School. Dr. Ho has participated in angiogenesis research, investigating causes and treatment for common retinal disorders.
 Sejal Shah M.D. is a board-certified, fellowship-trained Retina Specialist. Dr. Shah received her medical degree from the University of South Florida. She began her postgraduate training with an internship in medicine at UCLA, followed by ophthalmology training at the University of South Florida. She went on to complete a fellowship at the prestigious Bascom Palmer Eye Institute, specializing in the diagnosis and treatment of retinal disorders. Dr. Shah also earned a B.S. degree with honors in Nutritional Science from the University of Florida. Dr. Shah brings her expertise as a medical retinal specialist with skills in managing and treating vitreoretinal pathology which including age-related macular degeneration and diabetic retinopathy. Her research has appeared in publications such as Ophthalmic Surgery, Lasers, and Imaging Retina; Clinical Ocular Oncology; Survey of Ophthalmology; International Ophthalmology Clinics; and Survey of Ophthalmology. In her spare time, she enjoys spending quality time with her family and friends, traveling, and trying to keep up with her twin boys.
Sejal Shah M.D. is a board-certified, fellowship-trained Retina Specialist. Dr. Shah received her medical degree from the University of South Florida. She began her postgraduate training with an internship in medicine at UCLA, followed by ophthalmology training at the University of South Florida. She went on to complete a fellowship at the prestigious Bascom Palmer Eye Institute, specializing in the diagnosis and treatment of retinal disorders. Dr. Shah also earned a B.S. degree with honors in Nutritional Science from the University of Florida. Dr. Shah brings her expertise as a medical retinal specialist with skills in managing and treating vitreoretinal pathology which including age-related macular degeneration and diabetic retinopathy. Her research has appeared in publications such as Ophthalmic Surgery, Lasers, and Imaging Retina; Clinical Ocular Oncology; Survey of Ophthalmology; International Ophthalmology Clinics; and Survey of Ophthalmology. In her spare time, she enjoys spending quality time with her family and friends, traveling, and trying to keep up with her twin boys.

